There are no items in your cart
Add More
Add More
| Item Details | Price | ||
|---|---|---|---|
Prevention and treatment of Delirium
Wed Sep 17, 2025
This guideline from the American Psychiatric Association (APA), aims to enhance the quality of care for patients with delirium and prevent its development in at-risk individuals. Delirium is a significant and often unrecognized psychiatric condition, with prevalence rates ranging from 23% in medical inpatient units to 75% in mechanically ventilated ICU patients. It imposes a substantial economic burden, with estimated direct healthcare costs in the U.S. reaching billions annually due to prolonged hospital stays, rehospitalizations, and increased personnel time. Delirium is also associated with significant morbidity and mortality, increasing the risk of death, longer hospital and ICU stays, cognitive dysfunction, functional decline, and psychosocial distress for both patients and caregivers.
The guideline focuses on evidence-based non-pharmacological and pharmacological interventions for adults, grounded in DSM-5-TR diagnostic criteria. It excludes delirium related to alcohol or sedative withdrawal due to its distinct etiology and management. The development process adhered to rigorous standards, utilizing a systematic review of literature through July 2021 and employing the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach to rate the strength of guideline statements and evidence. The Guideline Writing Group (GWG) determined recommendations through a modified Delphi method, considering benefits, harms, patient preferences, and the strength of supporting evidence.
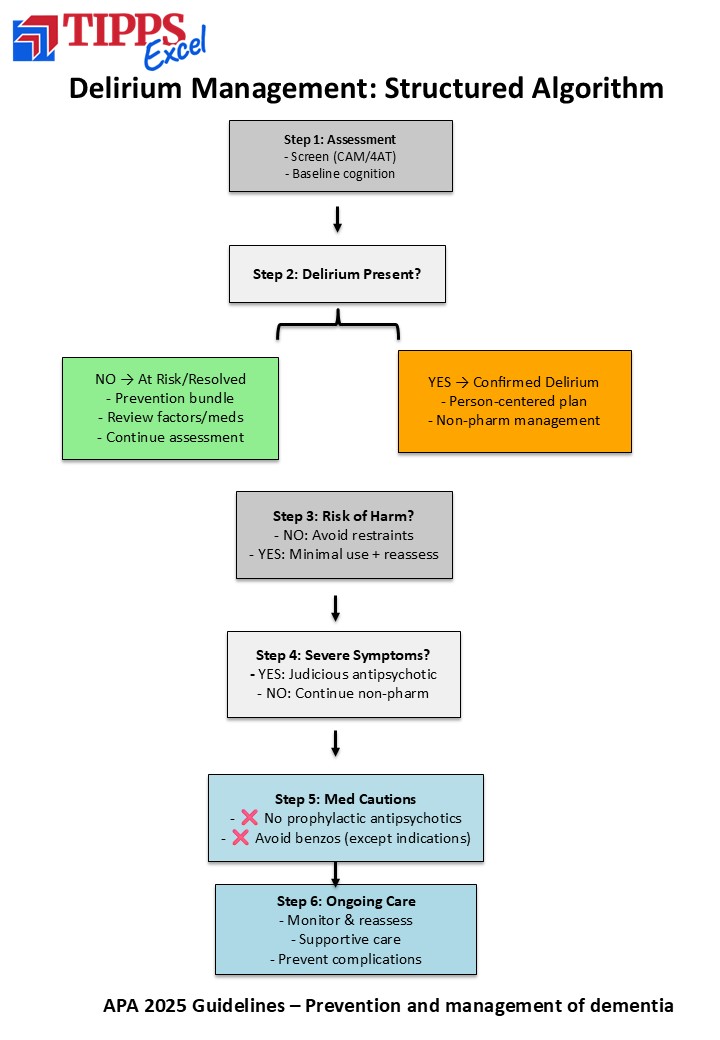
Key recommendations emphasize structured assessment for delirium, determining baseline neurocognitive status for accurate interpretation, and a detailed review of predisposing or contributing factors. A comprehensive medication review is crucial to identify and adjust medications that may contribute to delirium. For interventions, the guideline strongly recommends multi-component nonpharmacological approaches for both prevention and management of delirium. Pharmacological interventions should be reserved for severe neuropsychiatric disturbances causing distress or risk of harm, after de-escalation and addressing contributing factors have failed. Specifically, antipsychotic agents are not recommended for preventing delirium or hastening its resolution, though they may be used judiciously for acute agitation. Benzodiazepines are generally discouraged unless there is a specific indication, such as alcohol withdrawal or catatonia, due to potential adverse effects and worsening of delirium. Dexmedetomidine is suggested over other sedating agents for delirium prevention in patients undergoing major surgery or mechanical ventilation in critical care, and for sedating delirious patients on mechanical ventilation. Melatonin and ramelteon are not recommended for delirium prevention or treatment.
Finally, transitions of care are highlighted as critical junctures requiring detailed medication review, reconciliation, and reassessment of medication indications. Follow-up plans should include continued delirium assessments, evaluation of post-delirium consequences (e.g., PTSD, cognitive impairment), and psychoeducation for patients and caregivers.
10 Key Take-Home Points for Clinicians:
Link to the guideline document

Dr. Rishikesh Behere
Founder Admin, TIPPS